Translate
Subscribe to Blog via Email
Ronny Allan
Scope
This summary provides an overview of the types of therapy known for treating Neuroendocrine Cancer. They will have been approved at least by one national or regional approval agency, may not be available or approved in your own country; and may appear in clinical guidelines for the treatment of Neuroendocrine Cancer.
Clinical trials will not be covered, although it’s noted that some of the approved treatments listed may be in follow on trials either to prove new coverage or used in combination with another drug. For a list of clinical trials covered by the author, click here.
This summary will not include complementary or alternative treatment but may cover or overlap with experimental treatment.
Who recommends the best treatment for my condition?
Different types of doctors often work together to create a patient’s overall treatment plan that combines different types of treatments. This is called a multidisciplinary team (MDT) (in US the term “tumor board” can be used) and is very important for people with Neuroendocrine Cancer. These teams may comprise a variety of professionals, such as oncologists, surgeons, gastroenterologists, radiologists, endocrinologists, and many more as permanent members or co-opted for specific cases.
Treatment options and recommendations can depend on several factors, including:
- The type of Neuroendocrine Neoplasm (NEN) (a term covering well differentiated Neuroendocrine Tumour (NET) and poorly differentiated Neuroendocrine Carcinoma (NEC))
- Stage and grade
- The patient’s preferences and overall health
- The guidelines in place (e.g. ENETS/NANETS/UKINETS/CommNETS)
Treatment vs ‘Watch & Wait’

Watchful waiting or watch-and-wait, sometimes called ‘Active Surveillance, may be recommended for reasons that should always be explained. Ask why this approach is being taken and what the main risks are – you deserve to know. With this approach, the tumour is closely monitored with regular tests, including but not limited to:
- Imaging tests suitable for the type of NEN.
- Blood and urine tests as appropriate
- Physical examinations where applicable.
Surgery

Surgery is a common treatment for most NETs but less so with NECs. Surgeons, where possible, will try to remove all tumours and most localised NETs are successfully treated with surgery alone, often with curative intent. Additionally, the surgeon will usually remove some tissue surrounding the tumour to achieve a margin between cancerous cells and normal tissue. Check your post-operative biopsy report to see the details.
In cases of more extensive spread in NETs, a procedure called debulking surgery is sometimes recommended. Debulking surgery removes as much of the tumour bulk as possible (to an extent recommended in local guidelines) and may also provide some relief from symptoms caused by the tumour location and size or by hormonal secretions. Debulking surgery should not be considered curative. Surgery is not normally considered in NEC (poorly differentiated Neuroendocrine Carcinomas).
Often surgery is deemed not to be possible citing an “inoperable” tumour. Consequently, in these situations, the MDT will recommend another type of treatment. However, some surgeries can be very complex, sometimes risky, and one surgeon’s inoperable could be another’s operable. Many patients will seek a 2nd surgical opinion, always compare risks.
Surgery can be a very different experience from patient to patient. There are different types of NEN, different stages, different ages. You can read some of my surgery blog posts which contain links and videos with expert comment.
Surgery – to cut or not to cut. General surgery.
Small Intestine NETs – to cut or not to cut. The small intestine is not routine bowel surgery.
Small Intestine, Large Surgery. Patient experience plus expert reviews.
Pancreatic Neuroendocrine Tumours – surgical decisions – about surgery for Pancreatic NETs
For GammaKnife/CyberKnife/Stereotactic Radiosurgery (SRS), see Radiation therapy below. For NanoKnife see Ablation Techniques below
Somatostatin analogues

Somatostatin is a hormone that controls the release of several other hormones, such as insulin and glucagon. Somatostatin analogues are drugs similar to the hormone somatostatin and used to control the symptoms created by the hormone-like substances released by a NET. They may also slow the growth of a NET, although they do not generally shrink the tumours.
There are 2 somatostatin analogues used to treat NETs, octreotide (Sandostatin) and lanreotide (Somatuline). Octreotide is available in 2 forms: short-acting is given under the skin (subcutaneously) and long-acting is given as an intramuscular (IM) injection. Lanreotide is given as a long-acting deep subcutaneous injection. The most common side effects are high blood sugars, the development of gallstones, and mild digestive system upset, such as bloating and nausea. There’s actually a third one approved called Pasireotide (Signifor) but that is aimed at Acromegaly and Cushing’s Syndrome.
These drugs work better on somatostatin receptor positive tumours.
Who can get these drugs? It’s generally approved for those with locally advanced and metastatic cases of Gastroenteropancreatic NETs (GEP NETs) with or without syndrome. In many cases, this will be a first line therapy even administered before surgery in many cases, particularly those with a syndrome.
Read some of my blog posts about somatostatin analogues:
Lanreotide vs Octreotide – a side by side comparison.
Lanreotide – it’s calling the shots – my own experience with Lanreotide since 2010.
Peptide receptor radionuclide therapy (PRRT)

PRRT is the generic name for a nuclear therapy which uses a radioactive ‘peptide’ to attach to receptors on a tumour’s cell. With NETs, the somatostatin receptors which enable this treatment, exist in around 80% of patients. It’s a treatment not normally offered to poorly differentiated cases which are known not to express these receptors, although trials are ongoing.
The main treatment used is called Lutathera (the brand name) or Lutetium 177 (Lu177) which indicates the radioactive isotope used to attack tumour cells when combined with a somatostatin analogue variant which leads the payload to the tumour cells due to its known binding effect.
Who can get these drugs? The treatment is currently only approved for somatostatin receptor positive Gastroenteropancreatic NETs (GEP NETs). Different healthcare systems may have different patient selection criteria.
Read more here.
Targeted therapy

Targeted therapy is a treatment that targets the tumour’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of tumor cells while limiting damage to healthy cells.
Not all tumors have the same targets. The main ones in use to treat NETs involve mammalian Target of Rapamycin (mTOR) inhibitors and Tyrosine Kinase Inhibitors (TKI). There are several new targeted therapies in the clinical trial pipeline, so it’s worth taking a look at the link above to see more on this type of therapy.
The two main targeted therapies currently in use are:
Everolimus (Afinitor) is a targeted therapy, an mTOR inhibiter approved for the treatment of advanced non-functional NETs of the GI tract, lung, and pancreas. This drug can help slow down the growth of these tumours in some patients. Read more here.
Sunitinib (Sutent) targets a protein called Vascular Endothelial Growth Factor (VEGF), is approved for the treatment of advanced pancreatic NETs. Read more here.
Who can get these drugs? It’s generally approved for those with advanced and nonfunctional cases of Gastroenteropancreatic NETs (GEP NETs) but in the case of Sunitinib, only for pancreatic NETs.
These drugs are not dependent on somatostatin receptors.
Liver-directed treatment

If cancer has spread to the liver, the treatments below may be used at some point. These procedures are usually performed by an experienced interventional radiologist and may require an overnight hospital stay.
- Liver Embolization. NETs are known to be highly vascular, that is they live on blood supply. Tumour embolization is a procedure to shrink a liver tumour by cutting off its blood supply. The doctors put a thin, flexible tube, called a catheter, into an artery near your groin or in your arm. He or she guides the catheter into the liver artery (the hepatic artery) that supplies blood to the tumour. So, the theory is if you block the blood supply to a tumour, the tumour will reduce or die. It’s a procedure carried out by an interventional radiologist – it’s very much image guided. Other countries may use other appropriately trained personnel and they may have different names. There are essentially 3 types of liver embolization
Bland – Often known as Hepatic Arterial Embolization (HAE) or TransArterial Embolization (TAE). The technique is as described above.
Chemo – Transarterial Chemo Embolization (TACE). As per the bland type but they add some chemo (normally Fluorouracil (5-FU) but could be different depending on where you are). There is currently some debate about the actual advantages of that over bland.Radioembolization – Transarterial Radio Embilization (TARE). Also often called selective internal radiotherapy (SIRT), uses tiny radioactive beads (microspheres). It damages the blood vessels to the tumour so that it can’t get the nutrients it needs, and the radiation given off by the SIRT beads damages the cancer cells and hopefully stops them growing. The radiation used is mostly always Yttrium 90 or Y90. (Should not be confused with the Y90 version of Peptide Receptor Radio Therapy (PRRT) which is a different type of treatment and for the whole body).
Read more here.
Ablation Techniques
Radiofrequency ablation (RFA) and microwave ablation (MWA) use heat to destroy cancer cells or tumours (more than just the liver). The heat is supplied by electrical currents passed through a special needle placed directly into the liver. This may also be known as a percutaneous ablation. RFA/MWA is undertaken by doctors with special experience, and it may not be available at all treatment centres.
Cryoablation for cancer is a treatment to kill cancer cells with extreme cold. During cryoablation, a thin, wand-like needle (cryoprobe) is inserted through your skin and directly into the cancerous tumour. A gas is pumped into the cryoprobe in order to freeze the tissue. Then the tissue is allowed to thaw. The freezing and thawing process is repeated several times during the same treatment session.
Cryoablation for cancer may be used when surgery isn’t an option. Cryoablation is sometimes used as a primary treatment for:
- Bone cancer
- Cervical cancer
- Eye cancer
- Kidney cancer
- Liver cancer
- Lung cancer
- Prostate cancer
Cryoablation is also used to relieve the pain and other symptoms caused by cancer that spreads to the bone (bone metastasis) or other organs.
Cryoablation for cancer may also be called percutaneous cryoablation, cryosurgery or cryotherapy.
Irreversible electroporation also known as IRE, is a non-thermal ablative technique used to destroy cancer cells. It is a relatively new technique that has been used in medicine for over a decade, and its use is not widespread, as research is still being done into its efficacy. It is potentially a way to stop the growth or even reduce the size of cancer and prevent it from spreading (metastasis). The most well known version is branded under the name of Nanoknife® Today, the cancer most commonly treated with IRE is stage III pancreatic cancer. It can also be used in some cases for liver cancers (colorectal liver metastases, hepatocellular carcinoma (HCC), and neuroendocrine tumours) that cannot be treated with surgical resection (liver resection). Some urological cancers including prostate cancer and renal cell cancer may also benefit from treatment with IRE. IRE is based on pulses of electrical energy delivered between two electrodes. These electric pulses affect the membranes (outer surface) of the cancerous cells, changing the existing cellular membrane potential. This results in nanoscale (tiny) defects in the lipid bilayer of the membrane, which disrupts the stability of the cells and leads to a phenomenon known as apoptosis – cell death controlled by the body itself. The extent of cell damage and death depends on the amplitude, duration, frequency and number of pulses applied. Because IRE causes cell death through apoptosis, structures formed by proteins, such as vascular elastin and collagenous structures, are not affected, and therefore surrounding blood vessels are preserved. This allows for the ablation of malignancies (cancers) that are surrounded by these structures, which is typically the case for locally advanced pancreatic cancer. Unlike thermal-induced methods, such as microwave and radiofrequency ablation, which result in fibrosis and scarring, the apoptotic cells are phagocytosed (destroyed) by cells of the immune system and replaced by innate cellular degeneration. This treatment is not widely available.
Other less common methods
There are several other ablation techniques used worldwide: including Interstitial laser ablation and high-intensity focused ultrasound (HIFU).
Read my Ablation Blog
Includes the world’s first to use a recently FDA-approved ablation technology that can destroy large liver tumours.

Chemotherapy

Chemotherapy (chemo) is the use of drugs to destroy cancer cells, usually by keeping the cancer cells from growing, dividing, and making more cells. When people talk about “Chemo”, particularly patients and caregivers, they will anticipate this being the cytotoxic type of therapy commonly associated with toxic side effects including hair loss as the most well-known one. To a certain extent, this is accurate but worth pointing out that some chemo is more toxic than others (but still necessary depending on cancer type), some chemo is oral (tablet form) and not everyone suffers hair loss, and side effects usually go away after treatment is finished. Chemotherapy is normally administered via intravenous route (IV) but there are also oral (tablet) forms and may also be injected through a catheter (thin tube) directly into the abdominal cavity. This is called intraperitoneal (IP) chemotherapy. The latter is only for specific areas of anatomy.
Who gets Chemo in Neuroendocrine Neoplasms (NEN)?
There’s a longstanding myth in patient groups that “it doesn’t work with NETs”. This is only partly true. It is known not to be sufficiently effective with low grades (but still may be given in certain scenarios), it does not appear to like its slow cytokinetic growth. However, on the other end of the spectrum, it’s normally a first-line treatment for poorly differentiated Neuroendocrine Carcinomas.
It may also be a strong option for well-differentiated Grade 3 NETs and in certain scenarios for Grade 2 NETs.
Chemo types:
Platinum-based drugs (informally called platins) are chemotherapeutic agents used to treat many types of cancer including Neuroendocrine where it is tends to be exclusively for poorly differentiated Neuroendocrine Carcinoma. These drugs are used to treat almost half of people receiving chemotherapy for cancer. Commonly used chemo includes Cisplatin, Oxaliplatin, and Carboplatin.
Other Cytotoxic chemo include:
- Fluorouracil (5-FU),
- Streptozotocin (Zanosar)
- Irinotecan (Campto)
- Paclitaxel (Taxol)
and the oral (tablet) versions:
- Capecitabine (Xeloda),
- Temozolomide (Temodal),
- Etoposide (Etopophos, Vepesid)
Known combos used in NENs.
Cisplatin and Etoposide appear to be the most commonly used combo for high grade.
Capecitabine (Xeloda) and Temozolomide (Temodal) (CAPTEM) are used in cases of Grade 2 and Grade 3 NET but also listed as a second- or third-line treatment for NEC. Read more about CAPTEM by clicking here.
FOLFOX. Also known as Oxaliplatin de Gramont or OxMdG, which means modified Oxaliplatin de Gramont. It is made up of folinic acid (also called leucovorin, FA or calcium folinate), fluorouracil (5FU) and oxaliplatin.
FOLFIRI. Also known as irinotecan de Gramont or irinotecan modified de Gramont. It includes folinic acid (also called leucovorin, calcium folinate or FA), fluorouracil (5FU) and irinotecan.
Oxaliplatin and capecitabine (XELOX) Oxaliplatin and capecitabine is a chemotherapy combination known as XELOX. This combination might also be called CAPOX, CAPE-OX or OxCap.
FCarboSt. A combo of Fluorouracil, Streptozocin and Carboplatin. Use may be limited to Royal Free Hospital London. I would love to hear from others.
XELIRI or CAPIRI. Capecitabine and Irinotecan.
Read more about chemotherapy here.
Immunotherapy
Immunotherapy is designed to boost the body’s natural defences to fight the tumour. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function. Sometimes it is called biologic therapy.
There’s actually been an immunotherapy drug used in Neuroendocrine Neoplasms for some time and some of the long-term patients may have heard of it or have had it administered. Known as Interferon alpha (IFNα) it helps the body’s immune system work better and can lessen diarrhea and flushing. It may also shrink tumors. I still see this listed in some texts but less so recently, probably due to low efficacy and high toxicity.
When people talk about Immunotherapy today, they really mean the new drugs. While there are many clinical trials (some of which have already been declared not suitable), only two Neuroendocrine Neoplasms have at least one modern Immunotherapy drug approved:
- Merkel Cell Carcinoma has Pembrolizumab (Keytruda) and Avelumab (Bavencio).
- Small Cell Lung Cancer (SCLC) has Atezolizumab (Tecentriq) in combination with carboplatin and etoposide for extensive stage along with Nivolumab (Opdivo) for third-line treatment of metastatic SCLC.
Worth also mentioning that Pembrolizumab (Keytruda) is also approved to treat adult and pediatric patients with unresectable or metastatic solid tumors that are tissue tumor mutational burden (TMB) –high (≥10 mutations/megabase) and have progressed following prior therapy and who have no satisfactory alternative treatment options. This is part of a more targeted use of immunotherapy looking at specific gene mutations that may be present in any cancer.
Immunotherapy is exciting, but we also need to be aware of the risks of taking the brakes off the immune system. We have seen and heard more and more stories about people with grim cancer diagnoses who became cancer-free after treatment with immunotherapy. This offers hope to those with cancer, but we need to be cautious when discussing immunotherapy. This treatment method is still new, and the cancer community is still learning about how it affects the body. An unfettered immune system may end up attacking healthy, functioning parts of a person’s body, causing unpredictable side effects that may be life-threatening EVEN if not treated early.
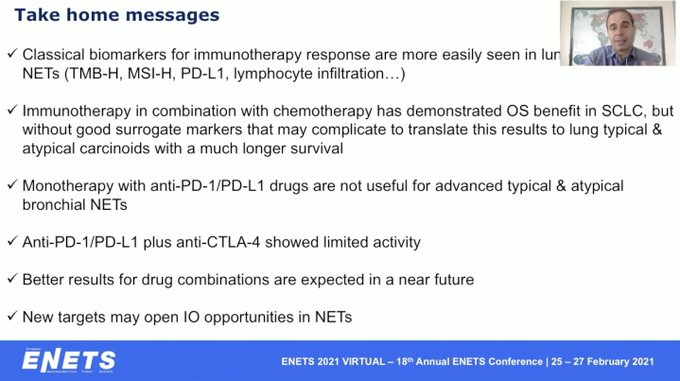
Nonetheless, our specialists continue to look for breakthroughs and this nice summary from ENETS 2021 is useful to those who are watching the immunotherapy story unfold.
Read more here. Given the amount of immunotherapy drugs in clinical trials, might be useful to take a look at all the posts I’ve written about clinical trials in the link above.
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to destroy tumour cells. A radiation therapy schedule usually comprises a specific number of treatments given over a set period of time. When people mention “radiation therapy” they normally mean something called “external-beam therapy“, the most common type given from a machine outside the body. Pepetide Receptor Radionuclide Therapy (PRRT) listed above is a totally different type of treatment. When people talk about Radiotherapy, they mainly think of “external beam” radiotherapy (EBRT) which is generally defined as a treatment using a special X-ray machine called a linear accelerator, EBRT delivers high-energy rays to tumors. The machine delivers radiation from any angle and shapes radiation beams to the contour of the tumor. The machine moves around the body without touching the patient, aiming radiation at the cancer. This type of radiotherapy is available in most hospitals. Only a small section will have the modern tools I will list below, although the widely deployed radiotherapy machines currently in service will still have some of these tools and technology, just not as advanced. It’s also worth pointing out that the more advanced tools and techniques are still at an experimental stage for many cancer types.
This is not a common treatment for most Neuroendocrine Cancers, particularly for lower-grade NETs. It is most often used as part of supportive or palliative care to relieve symptoms, such as pain, caused by cancer that has spread to the bone and other areas of the body. In terms of an anti-tumour approach, it’s more likely to be seen in difficult-to-reach areas and where precision is important.
Some types of focused EBRT target a tumor with higher, more precise doses of radiation while reducing damage to healthy tissue and nearby organs. As a result, modern EBRT may help reduce the risk of side effects associated with traditional radiation treatment. Many patients ask about other types of radiotherapy but there’s little information to suggest these are effective and/or widely used in Neuroendocrine Cancers.
Types of EBRT include:
- Image-guided radiation therapy (IGRT) is a technique used in SRS/SBRT which uses medical imaging to confirm the location of a tumour immediately before, and in some cases, during the delivery of radiation. IGRT improves the precision and accuracy of the treatment as it can allow for adjustments during treatment in areas of the body that are prone to movement, such as the lungs, and tumours located close to critical organs and tissues.
- Intensity-modulated radiotherapy (IMRT) uses linear accelerators to safely deliver precise radiation to a tumour while minimizing the dose to surrounding normal tissue.
- 3D conformal radiation therapy is a cancer treatment that shapes the radiation beams to match the shape of the tumour. Similar to IMRT in many ways in that they both target cancer while sparing healthy tissue.
However, I’ve included the following state of the art technology after noting that at least one patient had experienced one of these advanced types of radiotherapy/radiosurgery which tend to be under the general heading of Stereotactic radiosurgery (SRS)/Stereotactic body radiation therapy (SBRT)
Stereotactic radiosurgery (SRS)/Stereotactic body radiation therapy (SBRT).
- Stereotactic radiosurgery (SRS) is a type of radiotherapy to treat brain tumours. When it’s performed on the body rather than the brain, this procedure is sometimes called stereotactic body radiotherapy (SBRT) or stereotactic ablative radiotherapy (SABR). Uses 3-D imaging to determine the exact coordinates of a tumor. The highly focused gamma rays or x-rays then converge on the tumor to treat it. Because there’s no incision, SBRT isn’t a traditional type of surgery. Instead, SBRT uses 3D imaging to target high doses of radiation to the affected area. This means there’s very little damage to the surrounding healthy tissue. Like other forms of radiation, stereotactic radiosurgery works by damaging the DNA of the targeted cells. Then, the affected cells can’t reproduce, which causes tumors to shrink. The procedure uses many precisely focused radiation beams to treat tumors and other problems all over the body. SBRT is used to treat tumors in the lungs, spine, liver, neck, lymph node or other soft tissues. It’s an overarching term for many tools and techniques including
- Gamma Knife® is a radiation therapy that uses computerized treatment planning software to help physicians locate and irradiate small targets within the head and brain with very high precision. The treatment delivers intense radiation doses to the target area while sparing surrounding tissue. It can be used as a tool in SRS.
- Cyberknife® features a linear accelerator (linac) directly mounted on a robot to deliver the high-energy x-rays or photons used in radiation therapy. The robot moves and bends around the patient, to deliver radiation doses from potentially thousands of unique beam angles, significantly expanding the possible positions to concentrate radiation to the tumor while minimizing dose to surrounding healthy tissue. This robotic delivery and real-time image guidance have set the standard for delivery precision and enable stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) treatments for the full range of tumor types. It is used to treat conditions throughout the body, including the prostate, lung, brain, spine, head and neck, liver, pancreas and kidney, and can be an alternative to surgery or for patients who have inoperable or surgically complex tumors. CyberKnife treatments are typically performed in 1 to 5 sessions.
- Hadrontherapy. When the irradiating beams are made of charged particles (protons and other ions, such as carbon), radiation therapy is called hadrontherapy. The strength of hadrontherapy lies in the unique physical and radiobiological properties of these particles; they can penetrate the tissues with little diffusion and deposit the maximum energy just before stopping. This allows a precise definition of the specific region to be irradiated. The peaked shape of the hadron energy deposition is called Bragg peak and has become the symbol of hadrontherapy. With the use of hadrons the tumour can be irradiated while the damage to healthy tissues is less than with X-rays. These have some clear advantages even over protons in providing both a local control of very aggressive tumours and a lower acute or late toxicity, thus enhancing the quality of life during and after cancer treatment. Since the birth of hadrontherapy, more than 120,000 patients have been treated globally with hadrons, including 20,000 with carbon ions. In Europe, the interest in hadrontherapy has been growing rapidly and the first dual ion (carbon and protons) clinical facility in Heidelberg, Germany started treating patients at the end of 2009. Three more such facilities are now in operation: CNAO in Pavia, MIT in Marburg, and MedAustron in Wiener Neustadt are treating patients.
- Intraoperative radiation therapy (IORT) is an intensive radiation treatment that’s administered during surgery.
With credit to Radiopedia Info, Mayo Clinic, Hillman Cancer Center, Cyberknife, and CERN Enlight
I also wrote about small studies using SBRT to treat functional NETs and Lung NETs. You can read that here or click on the picture below:

Telotristat Ethyl (XERMELO)
Telotristat Ethyl is a significant introduction to the treatment of Carcinoid Syndrome diarrhea. It’s the first addition to the standard of care in more than 16 years and the first-time an oral syndrome treatment has been developed. The drug was previously known as Telotristat Etiprate but was changed to Ethyl in Oct 2016. ‘Etiprate’ was previously a truncation of ‘ethyl hippurate’. The brand name is XERMELO®
This drug is approved for the treatment of carcinoid syndrome diarrhea in patients inadequately controlled by somatostatin analogue therapy, i.e. it doesn’t replace somatostatin analogues – it is an additional treatment alongside and only when the diarrhea is caused by hormone oversecretion, i.e. it may not work to prevent post-operative diarrhea or other causal reasons.
In the simplest of terms, the drug is an inhibitor of the enzyme tryptophan hydroxylase (TPH). TPH is the rate-limiting enzyme in serotonin synthesis which converts tryptophan (an essential amino acid which comes from diet) to 5-hydroxytryptophan, which is subsequently converted to serotonin, one of the main causes of carcinoid syndrome effects including carcinoid heart disease. The trial data indicates that Telotristat ethyl significantly reduced the frequency of bowel movements.
Read more here
Summary
I wanted to provide a summary of the main treatments for Neuroendocrine Cancer without going into too much detail but still delivering something of use to the average patent. Not everyone will have access or need access to all of these treatments. I’m sure this is not an exhaustive list and I’m happy to listen to feedback on areas of both the quality and quantity of the information.
If you are in need of further information about your own treatment options, you should of course speak directly to your specialist. If you need to hear the experience of others who have gone through these treatments, you should post in my group. For those wishing to join, there’s a green button below with a link.
General Clinical Trials Disclaimer
Choosing to participate in a study is an important personal decision. Talk with your doctor and family members or friends about deciding to join a study. To learn more about this study, you or your doctor may contact the study research staff using the contacts provided in the clinical trials document. It’s very important to check the trial inclusion and exclusion criteria before making any contact. If you need questions, the articles here is very useful Questions to Ask About Clinical Trials | Cancer.Net
The inclusion of any trial within this blog should not be taken as a recommendation by Ronny Allan.
Top 10 Posts & Pages in the last 48 hours (auto updates) (Click the titles to read them)
Thanks for reading.
Personal Facebook. Like this page please.
Blog Facebook. Like this page please.
Awareness Facebook Like this page please.
Sign up for my newsletters – Click Here
My Diagnosis and Treatment History
Check out my online presentations
Check out my WEGO Health Awards
Check out my Glossary of Terms – click here
Please Share this post for Neuroendocrine Cancer awareness and to help another patient

A Review of April 2024 on RonnyAllan.NET
Here is the monthly summary of what we all achieved in April 2024. Something new, something blue and some borrowed too! Every share helps someone

I’m only as good as my last scan
“I’m only as good as my last scan”. I once received this comment in response to one of my posts. I thought it was a

Happy 10th birthday to my Blog Ronny Allan – Living with Neuroendocrine Cancer (RonnyAllan.NET)
On 29th April 2014, I release my first post entitled “What’s it all about” i.e. why on earth am I writing a blog! It was

Neuroendocrine – what’s that?
I once met some fellow cancer advocates and the conversation turned to what inspired us to ‘do what we do’. When it came to my

The trouble with the NET (Part 2) – Alternative Therapies – what’s the harm?
But it works, I read it on the internet! “But it works… I read it on the internet!”You may remember my article entitled The trouble

‘Chinese Dumplings’ and Neuroendocrine Cancer
Update of one of my posts from 2015 which was interesting in that year. This is not really about a treatment which is available everywhere

“An odd disposition of tumours” – less common metastases in Small Intestine and Pancreatic NETs
Every day is a learning day in NET! When I was diagnosed in 2010, my Oncologist sent me for a specialist scan that would help

Chemotherapy for Neuroendocrine Cancer
Edited and checked April 2024One of the unusual aspects of Neuroendocrine Cancer is that chemotherapy is not normally considered as a ‘standard of care’ or

Carcinoid vs Neuroendocrine
OPINION – There’s a constant debate regarding the validity of the term ‘Carcinoid‘. I’ve posted about this a few times and as far as I know,
A cup of tea
I would also mention those who contributed to my “Tea Fund” which resides on PayPal. You don’t need a PayPal account as you can select a card but don’t forget to select the number of units first (i.e. 1 = £4, 2 = £8, 3 = £12, and so on), plus further on, tick a button to NOT create a PayPal account if you don’t need one. Clearly, if you have a PayPal account, the process is much simpler
Through your generosity, I am able to keep my sites running and provide various services for you. I have some ideas for 2023 but they are not detailed enough to make announcements yet.
This screenshot is from every single post on my website and depending on which machine you are using, it will either be top right of the post or at the bottom (my posts are often long, so scroll down!)
Related
Discover more from Ronny Allan - Living with Neuroendocrine Cancer
Subscribe to get the latest posts to your email.














