Translate
Subscribe to Blog via Email
Ronny Allan
- Updated 11th March 2024 -
This section of my website has been published since 2015 but the most recent update to the World Health Organisation (WHO) Classification of Neuroendocrine Neoplasms is so significant, so gamechanging, that I have re-released the updated text. You may see these important publications called ‘Blue Books’.
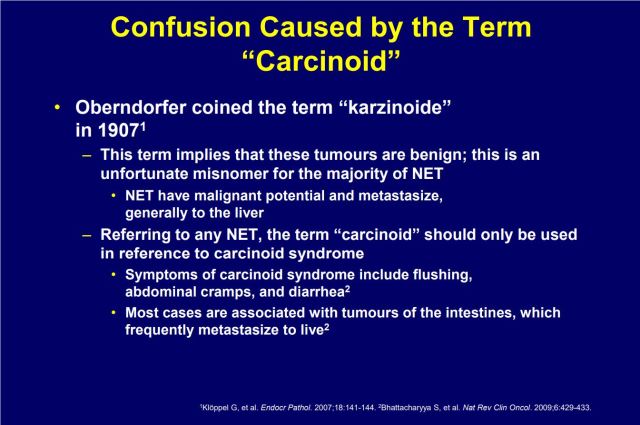
Words are very important in Neuroendocrine Neoplasms (NENs). Nomenclature has important meaning and context more than most other cancers due to the heterogeneity of this group of neoplasms. Grade and Stage are two factors inextricably linked to the nomenclature and while there have been less changes in these areas in the 2022 update, I have incorporated both in their own sections with enhancements to improve understanding.
Don’t be confused by the “2022” date as the major update is still in the printers as at 11th March 2024, so this is new information.
The WHO Classification of Endocrine and Neuroendocrine Tumours
Words are very important in NENs
To enable me to synchronise with the documented guidance, I’m going to use the following approved terms in this post and then provide an update of the key WHO 2022 changes below.
- Neuroendocrine Neoplasm (NEN) – all types of Neuroendocrine tumour of whatever grade and differentiation. Please note Neoplasm is another word for tumour.
- Neuroendocrine Tumour (NET) – all well-differentiated tumours, Grade 1,2 or 3 (an explanation of differentiation will be provided below).
- Neuroendocrine Carcinoma (NEC) – all poorly differentiated tumours. Neuroendocrine Carcinomas are by definition Grade 3. Other than Merkel Cell Carcinoma (a skin NEC), all NECs will have sub-types of large cell and small cell.
Notes:
1. The Thoracic WHO classification committee has decided not to implement a Grade 3 well differentiated Lung NET. Consequently, the above diagram does not apply to Grade 3 well differentiated Thoracic NETs (e.g. Lung and Thymus). They dissappointly left in the ‘carcinoid’ word, the only anatomical area in the entire WHO ‘blue book’ series to do so. Read more here. The former is up for review at the next iteration. I hope the latter is too!
2. Please note the addition of a Mixed Neuroendocrine Non-Neuroendocrine Neoplasms (MINEN) category. This is a situation where there is a mixed cell type comprising at least 30% of cells in each of the NEN component and the non-NEN component.
3. The terms “small cell” and “large cell” describe what cancer cells look like under a microscope. In NEN parlance, this only applies to NECs (including when they are the NEN component of a MINEN).
4. NECs are by default high grade (grade 3) and poorly differeniated. There is no need to prefix or sufffix these attributes to the term NEC. I do note that some pathologists not familiar with up to date NEN parlance, still use the term ‘carcinoma’ in pathology reports in relation to Grade 1 and 2 (and probably also to well differentiated Grade 3). You should always challenge that as a well differentiated patient given the potential differences in prognostics and treatments.
Background – The first ever WHO Classification of Endocrine and Neuroendocrine Tumours – 2022 (5th edition)
Previously, Neuroendocrine Neoplasms (NENs) were published in associated anatomy or body systems fashion, e.g. Small intestine NENs were contained in the Digestive System book, Pancreatic NENs were contained in the Endocrine ‘blue book’, and so on. The 2022 WHO Classification of Endocrine and Neuroendocrine Tumors is therefore a landmark publication. It replaces the 2017 Endocrine book but adds the digestive system 2019 ‘Neuroendocrine’ entries (effectively all gastoenteropancreatic NENs (GEPNENs) plus the various non-GEPNENs from several other books, grouping them together to form the 2022 landmark compilation.
Some progress towards this consolidation was actually made in the 2019 Digestive System by incorporating some endocrine NENs within this book (e.g. Pancreatic) effectively providing a GEPNEN book comprising 75% of all NENs. This new 2022 book takes that a huge step further.
However, I do not have the contents index for this large publication as it’s is still in the printers. In the absence of this confirmation, my main source of information will be cited below. Nonetheless, this is a major step forward in combining NEN classifications from the anatomical groupings (14 books in total) and should hopefully produce more accurate statistics from databases using the latest WHO classification system terms (that won’t happen overnight). The drivers for this change were outlined in a consensus document from 2017 where the authors stated “the classification of neuroendocrine neoplasms (NENs) differs between organ systems and currently causes considerable confusion. A uniform classification framework for NENs at any anatomical location may reduce inconsistencies and contradictions among the various systems currently in use. The classification suggested here is intended to allow pathologists and clinicians to manage their patients with NENs consistently, while acknowledging organ-specific differences in classification criteria, tumor biology, and prognostic factors“. The specialists were and still are on our side.
Sadly, some areas of the new combined classification have not changed in line with GEPNENs, I’m mainly talking about Thoracic NENs, e.g. Lung and Thymus. They will retain the archaic misnomer of “carcinoid” e.g. Typical Carcinoid and Atypical Carcinoid for well differentiated Grade 1 and 2 respectively. Additionally, they do not yet recognise the existence of a Grade 3 well differentiated NET. Instead, they will stick with the term “LCNEC with NET carcinoid-like features” but it is likely this to be synchronised in the next edition. Let’s hope they also ditch the archaic misnomer too. There are some other additions/changes which I will outline below.
Author’s Note: Although the overarching term for Neuroendocrine Tumours (NET) and Neuroendocrine Carcinomas (NEC) is “Neuroendocrine Neoplasms (NEN)”, the World Health Organisation (WHO) classification systems always use the term “tumours” across the board because ‘Tumour’ is a synonym of ‘Neoplasm’ and vice versa. The reason Neoplasm is used in Neuroendocrine Classification is to ensure the context and meaning of NET and NEC are not confused.
What’s new in the WHO Classification of Endocrine and Neuroendocrine Tumors – 2022 5th edition?
In addition to the major change outlines above, I offer you the following abstract summarising changes of note to patients and patient advocacy.
1. Neuroendocrine Tumours in Endocrine organs. The change from WHO Classification of Endocrine Tumours to the WHO Classification of Endocrine and Neuroendocrine Tumours is significant as most endocrine organs produce tumours which are already types of NEN.
2. New section on NENs in non-endocrine locations. This is recognition of the unique celluar properities of NENs in that it extends beyond the classic endocrine system to many other potential primary locations. This section includes (but not limited to) urogenital systems, head and neck, breast and skin.
3. Paraganglioma. Two unusual tumours that were initially thought to be paragangliomas have been reclassified as “paraganglioma like”.
a. One type of paraganglioma that mainly occurred in the duodenum was formerly known as “gangliocytic paraganglioma” but has now been recognised to be a composite gangliocytoma or ganglioneuroma with an epithelial duodenal NET. This lesion will now be renamed “composite gangliocytoma/neuroma and Neuroendocrine Tumour”. You will be pleased to hear this will be shortened to “CoGNET”.
b. A type of paraganglioma previously known as “cauda equina paraganglioma” has been reclassified as a “cauda equina Neuroendocrine Tumour”. I could not see an acronym shorterner.
As you can see, some changes are highly complex issues!
4. Biochemical testing. The authors emphasised the decreasing importance and role of biochemical testing from a diagnostic and surveillance point of view. I think we’ve all seen this in patient groups where some doctors will not even use these tests in clinical practice or at least place little value on their utility. There seems to be more emphasis on imaging in the absence of more efficient markers. They were mainly talking about Chromogranin A and 5HIAA, although they also (e.g.) cited the challenge in assessing the functional tumour status in patient with obesity, diabetes and gallstones with profound hypoglycaemia. They also discussed the new paradigm offered by molecular markers summarising that there needs to be a broad and dynamic dialogue between pathologists and clinicians to ensure accurate functional definition of endocrine and neuroendocrine tumours.
5. Molecular Markers. This is a glimpse of the future and a hugely complex issue. Therefore I will not dwell too long on it but I may write either a new post or a new section in here to delve into in patient speak (a challenge). Watch this space.
6. Small Pancreatic lesions. Previous known as “microadenoma”, the term “Neuroendocrine Microtumour” is now recommended (I suspect this is a move away from adenoma which has benign connotations and can be misconstrued in Neuroendocrine parlance).
7. New pancreatic functional tumour categories. They acknowledged the challenge of heritable genetic syndromes such as von Hippel-Lindau (VHL) and the Multiple endocrine neoplasia (MEN) syndromes with differing hormonal profiles. This was overlapped with a heightened awareness of the evolution of ectopic hormone production (e.g. the secretion of an organ specific hormone being secreted by a pancreatic NET), citing ectopic adrenocorticotrophic hormone (ACTH) or growth hormone-releasing hormone (GHRH) as a known issue leading to Cushing’s syndrome or Acromegaly respectively. The focus was previously on ACTH and Cushing’s syndrome but this has been expanded to include ectopic corticotropin-releasing hormone (CRH), ectopic parathyroid hormone (PTH) or parathyroid hormone releasing protein (PTHrP) and GHRH as above.
8. Neuroendocrine Carcinoma (NEC). Although frequently used today, the small cell and large cell subtypes are well documented within all NECs. However, there are exceptions where no subtypes exists, e.g. Merkel Cell Carcinoma.
9. Immunohistochemistry (IHC) stains. This is a highly complex issue but pathologists are learning all the time which patterns of IHC give the best indications of NENs and their likely source (primary site/type). I won’t repeat it here but I emphasise that the biopsy is a really important part of NEN diagnosis.
Reference: Rindi, Guido & Mete, Ozgur & Uccella, Silvia & Basturk, Olca & La Rosa, Stefano & Brosens, Lodewijk & Ezzat, Shereen & de Herder, Wouter & Klimstra, David & Papotti, Mauro & Asa, Sylvia. (2022). Overview of the 2022 WHO Classification of Neuroendocrine Neoplasms. Endocrine Pathology. 33. 1-40. 10.1007/s12022-022-09708-2.
The grading of Neuroendocrine Neoplasms

One of the most discussed and sometimes confusing subjects in patient groups are the staging and grading of Neuroendocrine Neoplasms (NENs). Mixing them up is a common error and so it’s important to understand the differences between the two, despite the apparent complexity.
Stage vs Grade
Although stage is discussed separately below, I think it’s important to compare them before talking in detail. As above, a lot of people get the two mixed up.
In the most basic of terms, stage is the spread or extent of cancer and grade is the aggressiveness of cancer. They are totally different attributes and an understanding of both is important as they are critical to predicting outcomes (to a certain extent) and guiding therapy. There is no correlation between the two, you can have the lowest grade with the highest stage (actually very common with NETs). If it helps, remember it this way – S for Stage (Spread), G for Grade (aGgressiveness).
The Stage is essentially worked out via scans and biopsy, particularly the size of the primary tumour and the depth of any invasion into nearby tissue/organs. It can be a complex analysis requiring many tests and can change. Although some signs and some testing can provide clues, working out the precise grade is currently only possible from a biopsy tissue sample.
As patients, we deal with many medical specialists during diagnosis and subsequent treatment. However, we rarely meet the pathologist who plays a critical role in the outcome. Precise diagnosis is what drives patient decisions and treatment. If the pathology is wrong, everything that follows might be wrong too. It’s a very important area.
If I was to make a list of questions for my specialist/Oncologist at diagnosis, it would include “What is the Stage and grade”. Moreoverm if I was in Grade 3 (High Grade), I would also want to know the ‘differentiation’ of my cancer in addition to the Ki67 and/or where applicable, the Mitotic Count.
Failure to make this clear in patient groups is going to cause enormous confusion for those posting or reading.
Why is differentiation important?
To fully understand grading, you also need to understand the concept of ‘differentiation’. In the most basic of terms, ‘differentiation’ refers to the extent to which the cancerous cells resemble their non-cancerous counterparts. This is an important point for high grade NENs because the differentiation of a high grade NEN could have an impact on both prognostics and treatment regimes.
Although there are 3 grades of NEN, there are two classifications of differentiation, and these become really important and only applicable at Grade 3.
Some of you may have heard the term ‘moderately differentiated’ which tended to align with an intermediate grade or Grade 2. However, please note that the term moderately differentiated as a classification was phased out in 2010 by WHO reducing from 3 differentiation levels to 2. Grade 2 is also defined as well-differentiated but based on different proliferative rate (see table).
Grading and Ki67/Mitotic Count
Grade is the aggressiveness of cancer – basically, how fast it’s growing. Neuroendocrine Neoplasms (NENs) are divided into 3 Grades depending on what range the Ki-67% measurement number lands in. With NENs, the differentiation (well or poorly) is very important when dealing with grade 3 as specialists now regard a well-differentiated tumour (i.e. a NET) with a Ki67 of less than 55% as important for outcomes and therapy decisions.
So, what is KI-67? It’s a nuclear protein associated with and may be necessary for cellular proliferation. It’s, therefore, an excellent marker to determine the growth fraction of a given cell population. The fraction of Ki-67-positive tumour cells (the Ki-67 labelling index) is often correlated with the clinical course of cancer. Pathologists normally need to count about a thousand cells to determine the percentage of cells that are Ki67 positive – thus why you see Ki67 expressed as a percentage. Zero percent is the lowest, 100% is the highest. Often, they add greater or less than signs depending on the sample involved, i.e. >5% or <5%.
There are other measurement systems in place, mainly Mitotic Count which tends to be more frequently used for Lung and Thymic NENs although often both measurement systems are given. Even in cases of small biopsies, the Ki-67 index can usually be determined but Mitotic rate counting requires a moderate amount of tumour tissue (at least 50 HPFs or 10 mm) and that may not be feasible for small biopsies. The Mitotic Count method may be mandated or preferred instead or in addition to Ki-67 for certain Lung and Thymic NET scenarios as it is said to be more helpful in distinguishing atypical from typical Lung and Thymic NETs, and for small and large cell lung Neuroendocrine Carcinomas (NEC).
Misc Grading Issues
The proliferative rate can be diverse in NENs, so sampling issues can limit the accuracy of grading. More substantial samples of tumour are therefore preferable for grading thus why the Ki-67 index is preferred for biopsies where large amounts of tissue may not be available. The distinction of low-grade from intermediate grade can be challenging when using small samples. A couple of interesting observations about NET grading which I spotted during my research and ‘forum watching’. You can have multiple primary tumours, and these might have different Ki-67 scores. Additionally, on larger tumours, Ki-67 scores can be different on different parts of the tumour. And something I know from my own experience; secondary tumours can have different Ki-67 scores than primary – even a different grade. In my own case, my liver secondary tumours were graded higher than my primary which according to my surgeon is in keeping with a clone of the disease having become more aggressive over time. Royal Free Hospital NET Centre indicates a person’s grade should be taken from the highest biopsy grade taken. This is a fairly complex area but a recent study published by the US National Institute of Health and many anecdotal comments made by NET specialists indicates that is a fairly common scenario.
All of the above is currently worked out via a biopsy.
The Staging of Neuroendocrine Neolasms
Now read about Staging of Neuroendocrine Neoplasms
Click here or on the picture below

Supplementary Information - additional areas of understanding
Additional areas of understanding:
NET vs NEC
Read my post by clicking here or on the graphic below:

Additional areas of understanding:
MANEC vs MiNEN
Added for completeness. This mixed and rare neoplasm type has traditionally been related to NEC but in 2017 the nomenclature change to a new term was necessary to reflect the fact that some of the tumours involved were not carcinomas or adenocarcinomas but rather were well-differentiated tumours or even adenomas (i.e. benign). Prior to 2017, known as Mixed AdenoNeuroendocrine Carcinoma (MANEC), they were renamed in the 2017 edition, to Mixed Neuroendocrine Non-Neuroendocrine Neoplasms (MiNEN).
MiNEN are neoplasms with two distinct neuroendocrine and non-neuroendocrine cell populations. They can be morphologically classified into three entities: collision, composite, and amphicrine MiNEN.
Diagnosis of MiNEN is usually facilitated by the presence of at least one well-differentiated component which may be the Neuroendocrine or Non-Neuroendocrine component. However, two ‘carcinomas’ are frequently reported. I guess this is the reason they moved from MANEC to MINEN in order to cover all scenarios.
The two components may be difficult to identify with conventional morphological techniques, particularly when they are poorly differentiated, and their identification may require additional immunohistochemical techniques. MiNEN usually originates from organs that contain neuroendocrine cells and in which “classical” NENs are known to develop, such as the pancreas, appendix, colon, and to a much lesser degree, the small intestine. Other locations in my source document include Oesophagus, Stomach, Biliary Tract and Gallbladder, Duodenum, Ampulla of Vater and Rectum.
There is a similar type in Lung NENs but the lung committee (2021) uses different terminology but only appear to talk about ‘intra lung’ combinations (click).
The WHO Classification of Neuroendocrine Neoplasms - the chronological changes since 2017
Background to the most recent changes in anatomaty based ‘blue books’
I think it’s useful to include the chronological changes since 2017 when the “WHO Neuroendocrine Revolution” began. I will keep here for reference.
Grading – Key WHO 2019 Changes (GEPNENs)
WHO Classifications of Cancer are published in something known in the medical world as “The Blue Book”. It’s important to understand the source of how all types of cancer (including Neuroendocrine) are named and graded, including any associated terms. This mainly comes from a World Health Organisation agency known as the International Agency for Research on Cancer (IARC). The “Blue Book” is in fact several books. Each book covers an anatomical system with the human body and Neuroendocrine Neoplasms are covered within each particular system – this is a topical point for Neuroendocrine Neoplasms given that they can appear anywhere in the body and often this causes confusion when describing cancers (e.g. we know the issues behind Pancreatic Cancer for example). There is a proposal for a single “Neuroendocrine” blue book but that has yet to come to fruition. However, the latest publication is “Digestive System” which covers most Neuroendocrine types so it’s a very useful update, and as you will see a milestone in resolving past nomenclature issues with our disease. The work behind the 2019 Digestive System follows on from the excellent work in the 2017 Endocrine update where the significant change from 2 to 3 grades of well-differentiated pancreatic NETs was a significant change. In fact, the 2017 pancreatic neuroendocrine update has been copied and pasted right into the pancreatic section of the 2019 digestive system book, effectively delivering a blue book that contains the vast majority of GEPNENs including those in the hepatopancreatobiliary organs (pancreas/bile duct/liver/gallbladder). Important to also point out that a very similar structure was presented in the 2017 Endocrine Organ blue book which included (but was not limited to) Neuroendocrine related tumours of the Pituitary, Thyroid, Parathyroid, Pheochromocytoma, Paraganglioma, and their associated hereditary syndromes. ENETS and many other regions adopted this for all types of Neuroendocrine Cancer (as a result of a proposal to do so), so the 2019 Digestive System is really a rubber-stamping of this change, but it also confirms one very important difference – the word “carcinoid” has been removed from the vocabulary, not before time and something I’ve been quite vocal about since 2015. Unfortunately many doctors and healthcare establishments still remain out of date.
So, what about other areas not included in GEPNENs? Please note there are still loose ends in some of the blue books, mostly Thoracic (Lung/Thymus). Hopefully, these blue books will be updated in the same way as the others for Neuroendocrine Neoplasms (or will be subsumed into the proposed Neuroendocrine blue book). But in the meantime, experts are proposing the nomenclature above be extended in advance of the blue book updates – this is covered in Neuroendocrine neoplasm update: toward universal nomenclature, © 2020 Society for Endocrinology 2020, Guido Rindi and Frediano Inzani. What this effectively means is that the term “carcinoid” is effectively now totally defunct other than the loose ends of Carcinoid Syndrome, Carcinoid Heart Disease and Carcinoid Crisis (problems I could resolve in 10 minutes if they would listen to me). In fact, one well known pathologist has been campaigning for the removal of the terms ‘carcinoid‘ since 2007
I’ll summarise the key changes from 2019 below for your convenience, but I need to cite the article here:
The 2019 WHO classification of tumours of the digestive system
Iris D Nagtegaal, Robert D Odze, David Klimstra, Valerie Paradis, Massimo Rugge, Peter Schirmacher, Kay M Washington, Fatima Carneiro, Ian A Cree, for the WHO Classification of Tumours Editorial Board. First published: 21 August 2019 – https://doi.org/10.1111/his.13975
- All well-differentiated GEPNETs now include Grade 3 alongside Grades 1 and 2.
- All poorly differentiated GEPNENs are now Neuroendocrine Carcinomas and are by default Grade 3 (the inference in the guidance is that there is no need to use the term high grade or Grade 3 in reference to Neuroendocrine Carcinomas as they have those attributes by default).
- Neuroendocrine Neoplasm is now the formal umbrella term for the grouping of well and poorly differentiated tumours.
- The term ‘carcinoid’ is no longer used in nomenclature for Neuroendocrine Neoplasms within the Digestive System blue book.
- Pancreatic Neuroendocrine Neoplasms will now appear in the Digestive System blue book, previously they were listed in the Endocrine Organ book.
- The molecular differences of well and poorly differentiated tumours have been added to assist pathologists in identifying them, e.g. Mutations in MEN1, DAXX and ATRX are entity defining for well differentiated tumours while Neuroendocrine Carcinomas (poorly differentiated) usually have TP53 or RB1 mutations.
- Poorly differentiated tumours are divided into Small Cell type (SCNEC) and Large Cell type (LCNEC).
- Last year the term “Goblet Cell Carcinoid” was changed to “Goblet Cell Carcinoma”. However, this type of appendiceal neoplasm has effectively been removed from the Neuroendocrine family as it’s now recognised to have a minor neuroendocrine component. This cancer type is now called Goblet Cell Adenocarcinoma of the Appendix.
- As per the previous content of this article, mixed tumours were renamed from Mixed AdenoNeuroendocrine Carcinomas (MANEC) are now named Mixed Neuroendocrine-Non-Neuroendocrine Neoplasms (MiNENs) – clearly they now have variable grades, variable mitotic rate/Ki67 and each component can be graded separately.
Grading – Key WHO 2021 Changes – Lung Neuroendocrine Neoplasms
Following the publication of the WHO 5th Edition of Thoracic (Lung/Thymic) Neuroendocrine Neoplasms in 2021, a new section will be added here – click here to see the differences
Pheochromocytoma/Paraganglioma
Previously, Pheochromocytoma/ Paraganglioma (PHEO/PGL) did not have an official grading regime, i.e. they were just benign or malignant. However, since 2017 and as reflected in the fourth edition WHO classification of Endocrine Systems, on the basis that all PHEO/PGL have some metastatic potential and have their own grading system, there are different classification systems for Pheochromocytoma and Paraganglioma These grades are based on molecular profiles (the future way for many cancers and the first time for a NET). They have a system of grading called GAPP (grading of adrenal pheochromocytoma and paraganglioma) and they are clustered into the metastatic risk (this is the beauty of molecular methods). So, they are different than regular NETs and they now have 3 differentiations, loosely related to grade. This change is complex and is covered in depth here.
Summary
A complex area and I hope I have condensed it sufficiently for you to understand enough for your purposes. Despite looking very scientific, it is not an exact science. There are many variables as there always are with Neuroendocrine disease. NENs can be very challenging for a pathologist even an experienced one who may not have encountered NENs before. However, it is an extremely important part of initial diagnosis and also when needed during surveillance. It is a vital tool used by Multidisciplinary Teams (MDT) in treatment plans and for prognostic purposes. If you need to learn further, I recommend this document:
References
- Rindi G, Mete O, Uccella S, Basturk O, La Rosa S, Brosens LAA, Ezzat S, de Herder WW, Klimstra DS, Papotti M, Asa SL. Overview of the 2022 WHO Classification of Neuroendocrine Neoplasms. Endocr Pathol. 2022 Mar;33(1):115-154. doi: 10.1007/s12022-022-09708-2. Epub 2022 Mar 16. PMID: 35294740.
- WHO Classification of Tumours Online
Additional Reading
You may benefit from reading these associated posts – click the blue titles:
Incurable isn’t always terminal
Disclaimer
I am not a doctor or any form of medical professional, practitioner or counsellor. None of the information on my website, or linked to my website(s), or conveyed by me on any social media or presentation, should be interpreted as medical advice given or advised by me.
Neither should any post or comment made by a follower or member of my private group be assumed to be medical advice, even if that person is a healthcare professional.
Please also note that mention of a clinical service, trial/study or therapy does not constitute an endorsement of that service, trial/study or therapy by Ronny Allan, the information is provided for education and awareness purposes and/or related to Ronny Allan’s own patient experience. This element of the disclaimer includes any complementary medicine, non-prescription over the counter drugs and supplements such as vitamins and minerals.
Top 10 Posts & Pages in the last 48 hours (auto updates) (Click the titles to read them)
Thanks for reading.
Personal Facebook. Like this page please.
Blog Facebook. Like this page please.
Awareness Facebook Like this page please.
Sign up for my newsletters – Click Here
My Diagnosis and Treatment History
Check out my online presentations
Check out my WEGO Health Awards
Check out my Glossary of Terms – click here
Please Share this post for Neuroendocrine Cancer awareness and to help another patient

A Review of April 2024 on RonnyAllan.NET
Here is the monthly summary of what we all achieved in April 2024. Something new, something blue and some borrowed too! Every share helps someone

I’m only as good as my last scan
“I’m only as good as my last scan”. I once received this comment in response to one of my posts. I thought it was a

Happy 10th birthday to my Blog Ronny Allan – Living with Neuroendocrine Cancer (RonnyAllan.NET)
On 29th April 2014, I release my first post entitled “What’s it all about” i.e. why on earth am I writing a blog! It was

Neuroendocrine – what’s that?
I once met some fellow cancer advocates and the conversation turned to what inspired us to ‘do what we do’. When it came to my

The trouble with the NET (Part 2) – Alternative Therapies – what’s the harm?
But it works, I read it on the internet! “But it works… I read it on the internet!”You may remember my article entitled The trouble

‘Chinese Dumplings’ and Neuroendocrine Cancer
Update of one of my posts from 2015 which was interesting in that year. This is not really about a treatment which is available everywhere

“An odd disposition of tumours” – less common metastases in Small Intestine and Pancreatic NETs
Every day is a learning day in NET! When I was diagnosed in 2010, my Oncologist sent me for a specialist scan that would help

Chemotherapy for Neuroendocrine Cancer
Edited and checked April 2024One of the unusual aspects of Neuroendocrine Cancer is that chemotherapy is not normally considered as a ‘standard of care’ or

Carcinoid vs Neuroendocrine
OPINION – There’s a constant debate regarding the validity of the term ‘Carcinoid‘. I’ve posted about this a few times and as far as I know,
A cup of tea
I would also mention those who contributed to my “Tea Fund” which resides on PayPal. You don’t need a PayPal account as you can select a card but don’t forget to select the number of units first (i.e. 1 = £4, 2 = £8, 3 = £12, and so on), plus further on, tick a button to NOT create a PayPal account if you don’t need one. Clearly, if you have a PayPal account, the process is much simpler
Through your generosity, I am able to keep my sites running and provide various services for you. I have some ideas for 2023 but they are not detailed enough to make announcements yet.
This screenshot is from every single post on my website and depending on which machine you are using, it will either be top right of the post or at the bottom (my posts are often long, so scroll down!)
Related
Discover more from Ronny Allan - Living with Neuroendocrine Cancer
Subscribe to get the latest posts to your email.















So is the best scenario for NETs, stage I, grade 1?
Also have you come across any data that says the biopsy sample used for the ki-67 test should be as recent as possible?
my team did the test Jan 2020, on samples kept from my original surgery back in 2011 ! ! (right hemi-colectomy).
surely the nets might be doing something quite different now, from how they were in 2011??
this doesn’t seem accurate way to do it?
cheers Ronny
Stage 1 Grade 1 is the best scenario for any cancer other than a benign condition.
I don’t believe there’s a push for continuous biopsy samples, although any post diagnostic surgery should be sampled. In the future, blood tests will function as biopsy (liquid biopsy)
Thank you this is every informative
[…] Neuroendocrine Neoplasms – Grade and Stage (incorporating WHO 2017 changes)/ […]
[…] Neuroendocrine Neoplasms – Grade and Stage (incorporating WHO 2017 changes)/ […]
My small intestine NETs was well-differentiated and therefore considered low grade but my TNM staging was 111b as it had metastasised to the lymph nodes. Despite open surgery to remove the tumour(s), I was put on a wait and see plan afterwards and given no dietary follow up, no access to a NET nurse, or any cancer nurse, no exercise plan and no support information. It’s been a 10-month journey to find my way with all this while trying to recover from horrendous surgery. Awful, but I’m getting there thanks to blogs like yours, to discovering the Australian Cancer Council, a NETs nurse at a capital city hospital who has allowed me to be on her closed network site to get info. It really is a joke! Top top it off because I present OK, my family think my cancer diagnosis must have been wrongly diagnosed and I’m cured. Sigh
https://polldaddy.com/js/rating/rating.js
I could write a blog post based on your comment! Clearly i wouldn’t mention your name or even your country if origin. TNM ….. what is 111b? Never seen it described like that …..
Thankyou again Ronny
Ronnie, this post is one I read again and again for reassurance! Your ability and willingness to make these diagnosis terms understandable is heart warming. You break the cancer mumbo jumbo down into phrases I can hold onto and find encouragement. Thank you.
Ronny, what percentage of patients are low, intermediate and high grade. Love your blog, the only one worth reading
You made me work with that great question. Information is sparse and I can see it is very location dependant. For example, nearly all NETS of the esophagus are Grade 3 but hardly any of the appendix are. I did find one study of 773 patients broken down to 16% grade 3, 10% grade 2, 74% grade 1. Thanks for the kind words.
Thanks Ronny it’s just so confusing you go from the one extreme,oh that’s nothing you just take a couple injections to that’s what killed Steve Jobs no wonder people are confused
Yes, it’s not easy, but stick with me, my aim is to help decode these things into something patients can understand.
Cheers Mate
Ronnie I see that you’re Scottish from the Facebook page.
I was born in Edinburgh although I live in NYC now . Missed my trip this year due to illness but I’ll be there next year at the Sheeps Heid having a pint
I’m a Dundee man. Now living in the south of England. I go up once a year, in fact just been up and drove the new route NC500 and went to the tattoo. See you in the Sheep’s Heidi 😃
Thank you. One comment: the link http://www.thenetalliance.com/pdf/NETs_Pathology_Report.pdf seems to be no longer available.
Thanks for letting me know. I recently criticised it for containing a major error to perhaps someone took my complaint seriously. Thanks again.
Thank you. As always.
Thanks tried to understand this for 5 years. Well done.
Reblogged this on Tony Reynolds Blog and commented:
If you are not some sort of hermit at some point in your life you are going to come in contact with a friend or relative who has cancer. This helpful blog that is looking at a particular type of cancer equips you with basic understanding of ‘Doctor Talk’ in the area of cancer, really worth spending a few minutes and reading!
Ronny, I have tried to blog about this exact thing multiple times but could not get a handle on it. Thanks for such a concise and clear summary! ~ Ed
I have to tell you Ed, my head hurt writing this!
This will be another Ronny Allan post that I will have to read more than one time and slowly at that! 😀
Ronny,
Excellent conversion of doctor speak to patient lanquage. I find that even people who have had the disease for a long time misunderstand and misuse these terms. Many physicians seem to misunderstand and misuse as well.
Good job!
Cy